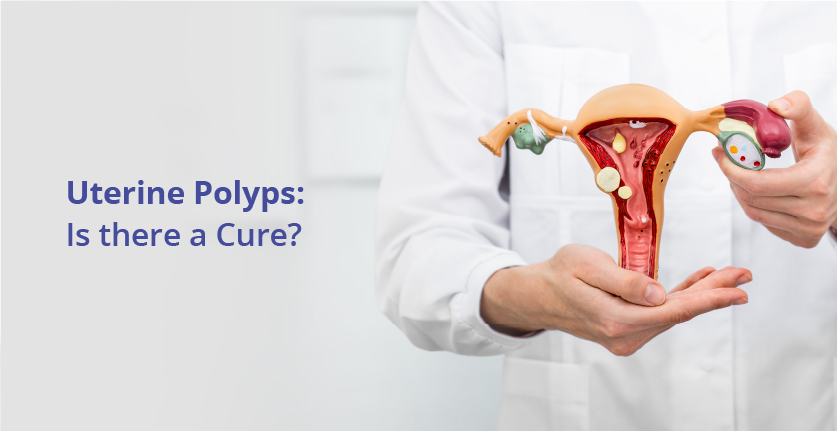
Everything About Uterine Polyps: Causes, Symptoms, Diagnosis, and Treatment
If you are bleeding between menstrual periods or have irregular menstrual bleeding, you might have uterine polyps. Uterine polyps might be associated with infertility. If you have uterine polyps and you’re unable to have children, removal of the polyps might allow you to become pregnant.
What are Uterine Polyps?
Uterine polyps are growths attached to the inner wall of the uterus that extends into the uterine cavity. Overgrowth of cells in the lining of the uterus leads to the formation of uterine polyps, also known as endometrial polyps. These polyps are usually noncancerous (benign), although some can be cancerous or can eventually turn into cancer (precancerous polyps).
Uterine polyps range in size from a few millimeters — no larger than a small seed — to several centimeters — ball-size or larger. They attach to the uterine wall by a large base or a thin stalk.
You can have one or many uterine polyps. They usually stay contained within your uterus, but occasionally, they slip down through the opening of the uterus (cervix) into your vagina. Uterine polyps most commonly occur in women who are going through or have completed menopause, although younger women can get them, too.
Risk factors of Uterine Polyps
Though the main cause of uterine polyps is identified as hormonal imbalance. But there are some risk factors that can lead to the formation of uterine polyps in the uterus-
- Women during perimenopause, menopause and post-menopause
- Being overweight
- A side effect of any hormone therapy
- A side effect of a drug or any other medicine used to treat other conditions
Complications of Uternie Polyps
Uterine polyps are benign and tiny growths of tissues. But in rare cases, these abnormal growths can turn cancerous. The formation of polyps is typically common during menopause. Some women may not experience any symptoms of uterine polyps. But in other cases, women with uterine polyps may face issues like infertility, miscarriage, and obstruction in the fallopian tubes.
What causes Uterine Polyps?
Hormonal factors appear to play a role. Uterine polyps are estrogen-sensitive and hence grow in response to circulating estrogen.
What are the symptoms?
The various signs that you might have uterine polyps are :
- Irregular menstrual bleeding — for example, having frequent, unpredictable periods of variable length and heaviness
- Bleeding between menstrual periods
- Excessively heavy menstrual periods
- Vaginal bleeding after menopause
- Infertility
Some women have only light bleeding or spotting; others are symptom-free.
Am I at risk of contracting Uterine Polyps?
You are at a risk of contracting uterine polyps if you belong to any of the below-mentioned categories:
- Being perimenopausal or postmenopausal
- Having high blood pressure (hypertension)
- Being obese
- Taking tamoxifen, a drug therapy for breast cancer
Diagnosis for Uterine Polyps:
There are multiple ways in which your doctor might help you find out if you have uterine polyps.
Transvaginal Ultrasound : A thin, wand-like device placed in your vagina emits sound waves and creates an image of your uterus, including its interior. Your doctor may see a polyp that’s clearly present or may identify a uterine polyp as an area of thickened endometrial tissue.
A related procedure, known as HSG (hysterosonography) involves having saltwater (saline) injected into your uterus through a small tube threaded through your vagina and cervix. The saline expands your uterine cavity, which gives the doctor a clearer view of the inside of your uterus during the ultrasound.
Hysteroscopy : Your doctor inserts a thin, flexible, lighted telescope (hysteroscope) through your vagina and cervix into your uterus. Hysteroscopy allows your doctor to examine the inside of your uterus.
Endometrial Biopsy : Your doctor might use a suction catheter inside the uterus to collect a specimen for lab testing. Uterine polyps may be confirmed by an endometrial biopsy, but the biopsy could also miss the polyp.
Most uterine polyps are noncancerous (benign). However, some precancerous changes of the uterus (endometrial hyperplasia) or uterine cancers (endometrial carcinomas) appear as uterine polyps. Your doctor will likely recommend the removal of the polyp and will send a tissue sample for lab analysis to be certain you don’t have uterine cancer.
How to treat Uterine Polyps?
Patience : Small polyps without symptoms might resolve on their own. Treatment of small polyps is unnecessary unless you’re at risk of uterine cancer.

Medication : Certain hormonal medications, including progestins and gonadotropin-releasing hormone agonists, may lessen symptoms of the polyp. But taking such medications is usually a short-term solution at best — symptoms typically recur once you stop taking the medicine.
Surgical Removal : During hysteroscopy, instruments inserted through the hysteroscope — the device your doctor uses to see inside your uterus — make it possible to remove polyps. The removed polyp will likely be sent to a lab for microscopic examination.
Way Ahead
If you think you have symptoms that match Uterine Polyps, do not panic but visit a trusted doctor. Sound medical diagnosis and advice is the best way forward. If you are found to have Uterine Polyps, medication or surgical removal can cure this condition. Uterine Polyps are generally non-cancerous and you will not need to worry about cancer. Also, once removed or treated, they do not recur in most patients.
Insert pitch for CKB
Transvaginal Ultrasound :

Hysteroscopy :